XFERALL Behavioral Health Collaborative Approach and 988 Crisis
For decades, it has been commonly understood that individuals experiencing a medical emergency shouldn’t wait for treatment. Treatment guidelines for individuals experiencing heart attacks, strokes and traumatic injuries prioritize rapid response. The medical community refers to the “golden hour” — the 60 minutes within which an injured or sick person should receive definitive treatment from the time of injury or onset of symptoms. If care is delayed beyond this hour, the risk of serious, long-term complications or death significantly increases. New systems of care, often regionalized, emerged to ensure that no precious time is lost in transporting, stabilizing, treating, and transferring patients.
Yet, for people experiencing a psychiatric or substance use emergency, a similar urgency coupled with system change hasn’t prevailed. Even in 2022, too many hospitals, crisis teams, first responders, and others needing to get people into behavioral health treatment quickly must rely on outdated, manual processes to locate clinically appropriate care, which cause critical delays in care. In their search for placement, clinicians are calling behavioral health facilities and programs one-by-one, leaving messages, faxing paperwork, and waiting for calls to be returned. The seemingly simple act of transferring a patient to behavioral health care is requiring clinicians to spend countless hours on repetitive administrative tasks that take them away from direct patient care.
The result is that, far too often, children, adolescents, and adults experiencing a behavioral health crisis wait hours or even days for placement in clinically appropriate therapeutic treatment. One study documents an average length of stay in the hospital emergency department for psychiatric admissions of 18 hours, compared to 5 hours for non-psychiatric admissions.1 Others have estimated average boarding times of between 6.8 hours and 34 hours for patients needing psychiatric treatment.2,3
Today, these wait times are likely even longer as the pandemic has made the ED boarding crisis worse in two ways. One, hospitals are at or beyond capacity with patients with COVID-19 and other serious physical conditions coupled with ever increasing staffing shortages. Two, the pandemic, and the associated anxiety, stress, and isolation, have contributed to an increased need for behavioral health care, particularly among children and adolescents. Children’s hospitals reportedly saw a 45 percent increase in pediatric self-injury and suicide cases between January and July 2021.4 In 2020, pediatric mental health-related hospital emergency department visits increased 24 percent for children ages 5-11 and 31 percent for older children and adolescents.5
XFERALL’s mission is to drastically save time for clinical staff and reduce the amount of time patients spend in EDs waiting for a transfer to the most appropriate care center by applying innovative technology solutions. The platform enables real- time communication so that clinicians needing to place a patient can request placement at as few or as many facilities as they choose; receive responses from facilities or programs that can accept and treat the patient; and share clinical information — all within minutes and within a single source. This coordinated approach allows caregivers and patients to be engaged in the decision-making process as well.
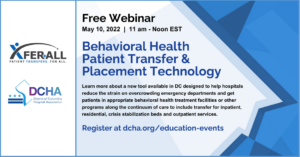
The District of Columbia Hospital Association and XFERALL, the nation’s leading mobile patient transfer platform, have entered a partnership that offers DC hospitals a new process for transferring acute and behavioral health patients to clinically appropriate health care facilities. To learn more, join us on May 10 for a free webinar, Behavioral Health Patient Transfer & Placement Technology, and learn about this program and how it can support improving access for patients in crisis.
1 Nicks BA, Manthey DM. The impact of psychiatric patient boarding in emergency departments. Emerg Med Int 2012; 2012: 360308.
2 Weiss AP, Chang G, Rauch SL, et al. Patient and practice-related determinants of emergency department length of stay for patients with psychiatric illness. Ann Emerg Med. 2012;60(2):162–71.
3 Tuttle GA. Access to psychiatric beds and impact on emergency medicine. Chicago, IL: Council on Medical Service, American Medical Association; 2008.
4 Pediatricians, Child and Adolescent Psychiatrists and Children’s Hospitals Declare National Emergency in Children’s Mental Health, October 19, 2021.
aacap.org/aacap/zLatest_News/Pediatricians_CAPs_Childrens_Hospitals_Declare_National_Emergency_Childrens_ Mental_Health
5 Ibid